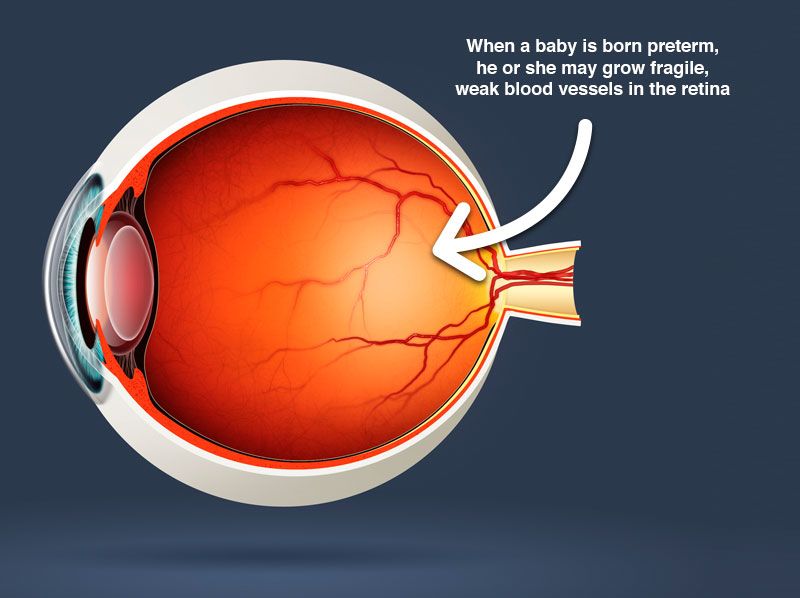
The fragile preterm infant is suddenly born into an environment so different from their safe and secure world in the womb. The neonatal intensive care unit (NICU) is their first home. This artificial and over stimulating world of bright lights, loud sounds, unpleasant and painful touch, unpleasant smell and taste disorganizes these vulnerable babies at a time which is critical for neuro development, both in terms of structure as well as function. This blog focuses on the tiniest and most vulnerable babies, but it is applicable to all preterm infants in general.
Adaptations made in the NICU help balance the needs of giving critically ill babies the highly specialized medical care necessary for their survival while protecting them from the challenges of their new surroundings. This has led to the emergence of developmentally supportive care. It is based on the concept that one should create an environment as similar as possible to that of the womb. Such an environment provides care and support to these babies, helping them to organize their state of mind, reduce negative impact and have an optimal development of their brain.
Developmentally supportive care comprises of:
- Protected sleep
- Pain and stress assessment and management (NICU can use scoring system to assess pain and respond accordingly)
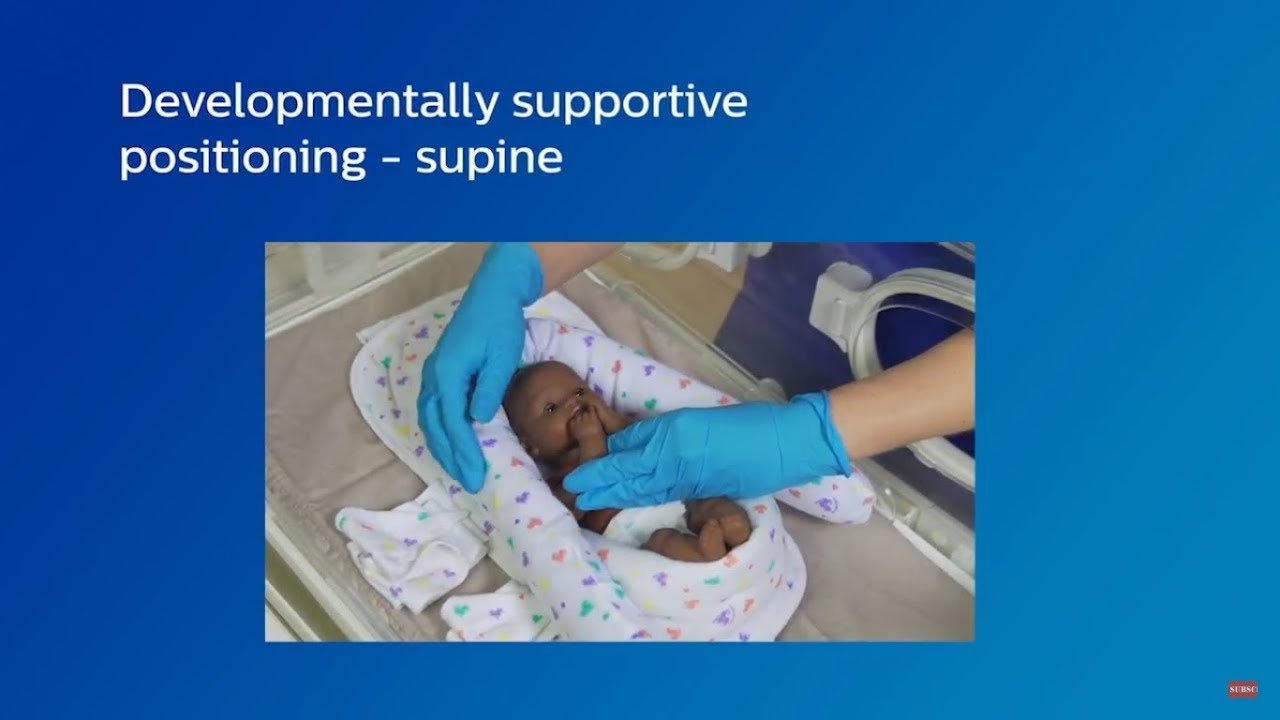
- Containment (gently placing baby in flexed position)
- Facilitated tucking (bringing body to middle)
- Swaddling (wrapping the infant in such a way that movement is restricted)
- Nesting (providing a boundary similar to that in the womb; thus the infant has a surface to touch)
- Providing a healing environment (minimize sound and light)
- Clustering activities
- Kangaroo care/ Skin to skin cuddles
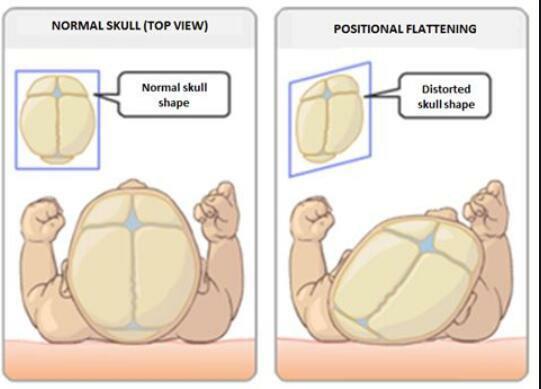
- Gentle positioning and skin care
- Non-nutritive sucking
- Scent cloth
- Oral immune therapy
- Involving family in all types of care
You can look at their behavioral cues to understand how they react to different sensory inputs. Does she like stroking, or constant pressure or just a touch? Does she dislike a particular type of activity? Ensure that your hands are clean nails are washed, you are not using strong scents or lotions and that your hand is warm before touching your little one. Remember to always talk first, then touch, then move.
Once it is understood that the infant is in a state of optimal readiness try to engage gradually. A caring exchange is accepted well by an infant and can be measured by improvement in their sleep-wake cycle and normal vital signs. Occasionally there is an improvement in respiratory parameters, heart rate and blood pressure. Depending on a baby’s ability to sustain a mutual relationship, the developmentally supportive care provider (parent/nurse) can begin their caring. This is known as ‘cue based care’.
If a baby is alert and has normal vital signs, it would be ideal for interaction. Whereas a baby who has frequent alarms going off on the monitor, squirming uncomfortably or crying might not be ready for interaction but can be comforted by being spoken to or hand hugging. Thus, care can be modified based on an individual baby’s needs. Just like interacting with an adult, one needs to be a gentle man/ gentle woman with a preterm baby. Remember, never tap or knock the incubator. Open and close the side ports gently. Never place any item on top of the incubator. Doing so would expose your little one to very very loud sounds.


Consider a trivial task like diaper change. While engaging in a developmentally supportive diaper change, consideration of light and sound levels within the immediate care area, positioning and comfort needs during the procedure, assessment of skin integrity and responses to handling, and whether or not the family wishes to participate in care should be always checked. To enable this care, single patient room concept has become popular in NICU. Although tremendous advances in neonatal care and the developmental support offered to high risk infants have been made, variability in practice remains a constant concern. The bedside nurse plays a vital role in determining the type and quality of developmentally supportive care offered to the infant.

The unit where I work, practices a beautiful concept of using a ‘scent cloth’. All mums who deliver extremely preterm neonates are given a small piece of sterile cloth to be placed on her bare skin. After a few hours that cloth is removed and placed in the vicinity of her infant in the incubator. This enables bonding of the tiny infants with their mum in a safe way. ‘Oral immune therapy’ is also a very important way to establish bonding and help enhance the successs rate of early feeding in extreme preterm infants. Very tiny amounts of expressed breast milk, as low as 0.2 to 0.5 ml is smeared on the infants lips or inserted into her oral cavity. This has proven to enhance short-term outcomes in tiny preterm infants.
Even in the very early days of life you should be allowed to touch your baby irrespective of their gestational age. Gentle foot massages can be a lovely parenting occupation. Especially because many of the sensory experiences to the feet are not pleasant in the NICU (Ex: pick, SpO2 probe application). Experiencing less pain is a real gain. Research shows that young adults with preterm birth history have differences in sensory processing compared to general population. You can read more about pain in NICU in my previous blog which was entirely dedicated to “Impact of early life pain”. There is also a blog on “Play and activity in the NICU” which you may find useful.
In the NICU, the neonatal team can support you based on your baby’s behaviour, medical status and development. Try skin to skin care with your infant for an hour or more every day. A 20 year follow-up of RCT shows larger volumes of total grey matter, basal nuclei and cerebellum in those who had received kangaroo mother care vs routine incubator care.
As your baby grows up, and transitions to lower level of support, an Occupational therapist can help you try breast feeding. Breastfeeding offers so many nutritional benefits, but it also creates the best sensory environment to love, learn and grow. And as you start your journey at home, remember to approach your baby from the middle. Being in the middle helps get hands to mouth, find a fist to suck on, feel comforted and look at you. The muscles in your baby’s face copy what you are doing. A parents face and voice is always the number one toy. Baby’s sensory needs are best met in the loving arms of parents. Smiles are everything. That look of love that little babies offer their mums and dads is called as ‘Primary Intersubjectivity’.
It is important for all NICUs to stop separating parents and babies. For preterm infants the single biggest influence on their neurodevelopmental outcomes are their parents. NICUs should always support families and never view a baby in isolation and this is the mantra of ‘Family centered care’.
You will gradually learn what your newborn is saying to you, because babies communicate with their behavior. Signs of sensitivity include yawning, sneezes and hiccoughs. If they experience too much sensory input they may need a moment to adjust. The ease with which parents hold a baby, shapes what love will feel like for that child for the rest of their life.
Have a lovely parenting experience you all..!